

Pathophysiology of ß2-adrenergic receptor, vascular dysfunction and hypoxemia
We described a disturbed interaction between the cardiovascular system and the skeletal muscle, where dysfunction of vascular and cardiac ß2AdR together with endothelial dysfunction of other causes plays a key role.

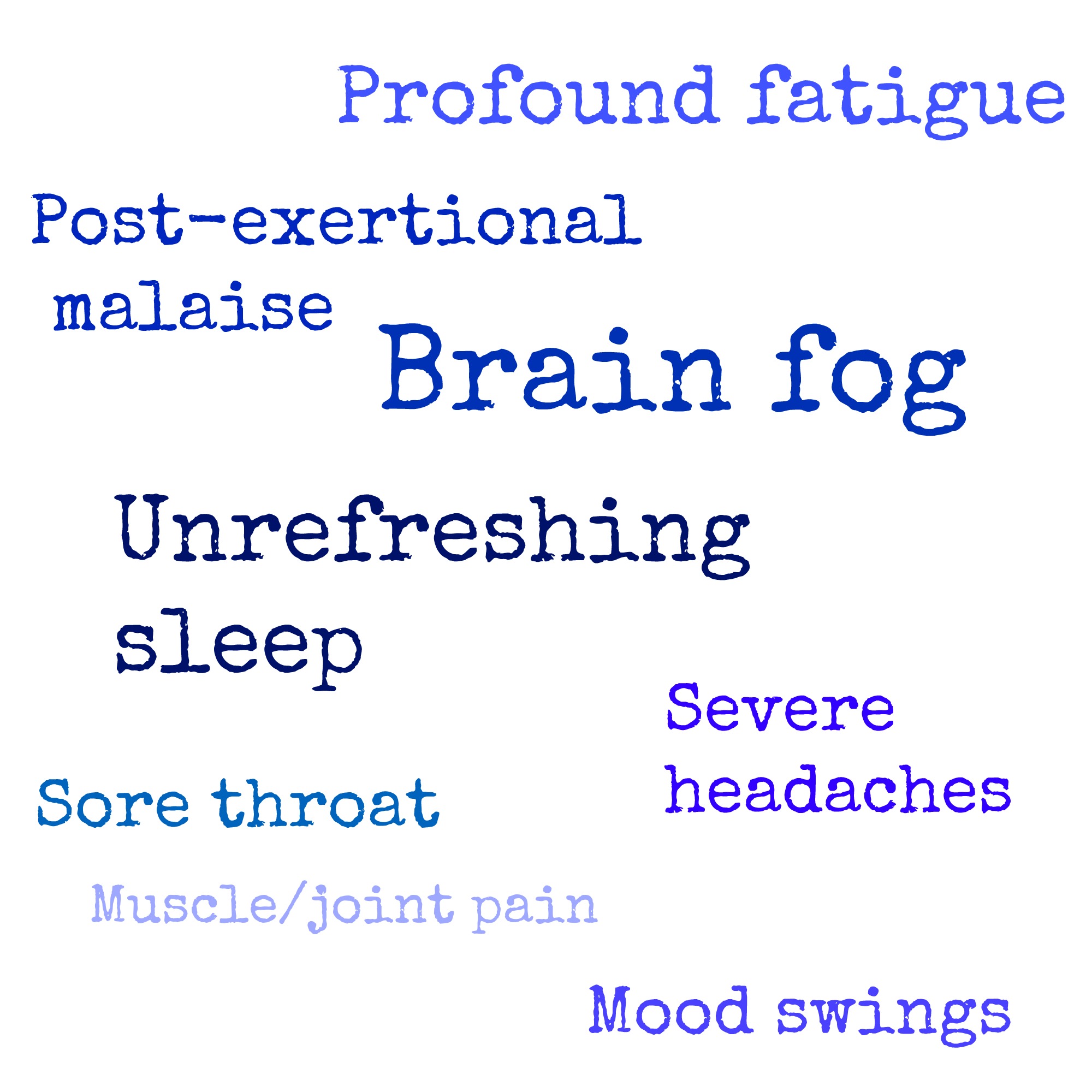
In a first hypothesis paper initially stimulated by the finding in ME/CFS patients of autoantibodies against ß 2-adrenergic receptors (ß2AdR) we hypothesized that ß2AdR dysfunction could be of critical importance in the pathophysiology of ME/CFS, see Textbox 1). This co-occurrence of seemingly unrelated symptoms and findings prompts to look for a unifying explanation (the most parsimonious explanation). Many symptoms are, however, not obviously explained by neurological pathology including the cardiovascular situation with orthostatic intolerance, hypovolemia and a low activity of the renin–angiotensin–aldosterone system (RAAS), or the impaired muscle function (reduced handgrip strength and fatigability) and energetic disturbance. This is based on neurological symptoms including mental fatigue, impaired cognition, psychomotor slowing, disturbed sleep, hypersensitivities to noise, light and smells, headache, pain and paresthesias and severe dysautonomia. ME/CFS is classified as a neurological disease. Very recent studies into post-Covid-19 syndrome (PCS) suggest that there is a broad overlap in symptomatology between both conditions. ME/CFS is often triggered by infections with various viruses, like EBV, enteroviruses, influenza virus, dengue fever and as a recent example Corona virus (SARS-CoV2). It presents with a confusing variety of symptoms ranging from neurological symptoms, fatigue, exertional intolerance with post-exertional malaise (PEM), chronic muscle pain, skeletal muscle and cardiovascular findings to complaints arising from many other organs.

Myalgic Encephaloymelitis (ME/CFS) or Chronic Fatigue Syndrome is a frequent and debilitating but still enigmatic disease. The Creative Commons Public Domain Dedication waiver ( ) applies to the data made available in this article, unless otherwise stated in a credit line to the data. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. It may also include coping techniques, and ways of managing your daily activities.Open AccessThis article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. It may include therapies to manage your symptoms, such as medicines to treat pain, sleep disorders, and other problems. You should work with your doctors to create a treatment program that best meets your own needs. There is no cure for CFS, so the goal of treatment is to improve symptoms. It is most common in women in their 40s and 50s, but anyone can have it. Your doctor has to rule out other diseases before making a diagnosis of CFS. There are no tests for it, and other illnesses can cause similar symptoms.


 0 kommentar(er)
0 kommentar(er)
